What Are The Requirements For A Patient To Have Robotic Mitral Valve Repair
Review Article on Minimally Invasive Cardiac Surgery
Robotic mitral valve surgery: a review and tips for safely negotiating the learning bend
Introduction
Mitral valve surgery has a long history of innovation, being at the leading edge of development of minimally invasive cardiac surgical (MICS) techniques for over ii decades at present. Recognition of the significant advantages of minimizing surgical trauma by reducing incision size and eliminating rib-spreading has resulted in a substantial increment in the number of minimally invasive cardiac surgical procedures being undertaken internationally, such that 54% of isolated mitral valve disease in Germany is now performed using minimally invasive (predominantly non-robotic) techniques (i). The benefits of MICS include less hurting, claret loss, shorter hospital stays, faster return to normal activities and improved cosmesis when compared to conventional sternotomy surgery. This is at the expense of consistently longer operative times that accomplish parity with increasing feel (2-5). Advances in MICS accept been facilitated by improvements in surgical techniques (e.g., Gore-Tex loops), instrumentation (shafted instruments), perfusion technology (thin-walled reinforced cannulae) and vision platforms (3D video stacks). Improvements have ensured that minimally invasive procedures are every bit constructive and durable as conventional surgery (half-dozen).
Potential advantages of robotic surgery over mini-mitral surgery
There are several disadvantages of video-assisted mitral valve surgery. Although the minithoracotomy peel incision is minor, usually iv–6 cm in most surgeons' easily, the intercostal incision is larger, probably 8–10 cm. Undercutting of the incision allows the ribs to spread wider with only a soft tissue retractor permitting surgery using direct vision which is more familiar and expeditious. Relatively few surgeons performing mini mitral surgery take mastered a totally endoscopic procedure. Robotic surgery using the da Vinci system (Intuitive Surgical, CA, U.s.a.) requires the surgeon to work completely endoscopically as the console is remote from the patient. A truly minimally invasive arroyo where the largest port incision is 20 mm or smaller tin can therefore be achieved (Figures i,2). We believe the faster recovery observed with robotic surgery when compared to mini-mitral surgery at our establishment is probably related to these factors, as well as the remote centering of the da Vinci arms ensuring that minimal pressure is placed on the intercostal bundles. Whether any reward in operative durations or patient benefit can be demonstrated in comparing to totally endoscopic mini mitral surgery using 3D vision platforms remains to exist clarified.

Effigy 1 The da Vinci Xi (reproduced with permission from Intuitive Surgical).

Effigy two The LEAR Technique (Lateral Endoscopic Approach for Robotics). A, admission port; E, endoscope port; L, left arm port; LA, left atrial retractor port; R, correct arm port.
Robotic surgery also provides a solution to the limited dexterity of endoscopic instrumentation (only 4 degrees of freedom combined with the fulcrum effect). This is frequently challenging for many cardiac surgical procedures, and the loss of depth perception if second video monitors are used only farther compounds operative difficulty. The robotic panel facilitates surgical virtual immersion into the operative field through 3D-Hard disk imaging, placing the surgeon inside the left atrium with a line of vision parallel to the flow of blood through the mitral valve (Figure 3). Finger and wrist movements are registered through sensors and translated into motion-scaled tremor-gratis movements fugitive both the fulcrum event and the musical instrument shaft shear forces common to long-shafted endoscopic instruments. Wrist-like articulations at the ends of micro-instruments bring the pivoting action of the instrument to the aeroplane of the operative field, improving dexterity in tight spaces and allowing truly ambidextrous suture placement.
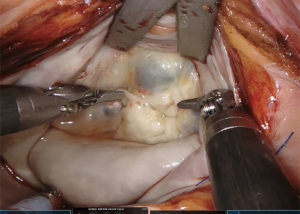
Figure three The operative view with the da Vinci.
Early development
Many of the pioneers of video-assisted or endoscopic mitral valve surgery were as well early on adopters of robotic technology, with Carpentier, Mohr, Chitwood and Potato leading the way (7-nine). The beginning robotic mitral valve repair was performed in May 1998 by Carpentier using an early epitome of the da Vinci articulated intracardiac "wrist" robotic device (vii). A week after, Mohr performed the first coronary anastomosis and repaired 5 mitral valves with the device (8). Grossi et al. (ten) of New York Academy partially repaired a mitral valve using the Zeus™ system (Estimator Move Inc., CA, USA) but no annuloplasty ring was inserted. Iv days later, in May 2000, Chitwood performed the first complete da Vinci mitral repair in North America. Two Food and Drug Administration (FDA) trials subsequently led to approval in November 2002 of the da Vinci organization for mitral valve surgery (11,12).
Since and so, the United states has seen the greatest uptake of robotic cardiac surgery, probably due to the competitive nature of their healthcare organization. Instance numbers plateaued at approximately one,700 robotic mitral valve procedures per year from 2009 to 2022 (xiii). However, robotic surgery in Europe is making a resurgence, with a steep increment in the annual number of cases every bit new centres accept upwards this pioneering engineering science. In this review, we volition evaluate the current evidence for robotic mitral valve repair.
Operative outcomes
Ane of the key challenges when introducing whatsoever less invasive technique has been the ability to demonstrate at least equal if non amend results when compared to a aureate standard of median sternotomy. Randomised controlled trials comparison operative techniques confront tough hurdles. For instance, appropriate blinding of patients and agreement of surgeons to use sternotomy in institutions with well-established robotic programmes and favorable outcomes. When well-informed patients are faced with the 50% possibility of being randomised to a sternotomy in one institution, they are likely to search for their desired handling elsewhere. As a effect, evaluation of robotic mitral valve surgery is based largely on single center experiences supplemented by large database analyses with propensity matching.
Mortality
Patients entered into robotic programmes accept certainly been more selected than those undergoing sternotomy. Avoidance of retrograde femoral arterial perfusion in patients with significant aortovascular disease and the exclusion of patients with severe mitral annular calcification has contributed to robotic cohorts which are younger and with fewer co-morbidities than sternotomy groups (14,15). Unmatched comparisons accept therefore not unsurprisingly shown a lower bloodshed for robotic mitral valve patients, which fails to retain significance when matched comparisons are fabricated (fourteen). In a propensity score matched analysis of 631 pairs of patients, Paul et al. (xiv) establish no meaning difference for in-hospital mortality, complications, or composite outcomes in unadjusted or multivariable analyses, betwixt patients undergoing robotic-assisted and non-robotic mitral valve repair. Nonetheless, what remains overwhelmingly consistent is an operative mortality with robotic mitral valve repair of <ane% in large series, with some centres achieving goose egg mortality (sixteen-19).
Valve repair rates and durability
An added measure of confidence in the technology can be derived from the knowledge that benefits are accrued without compromising valve repair rates or the immovability of mitral valve repair. In a regional Social club of Thoracic Surgeons (STS) database analysis from 2022 to 2022, Hawkins et al. demonstrated a higher charge per unit of repair in robotic procedures when compared with sternotomy despite like rates of degenerative affliction (20). Interestingly, in this report, which besides matched patients to a mini-thoracotomy approach, repair techniques varied little between mini and robotic approaches, whereas sternotomy was associated with a greater number of leaflet resections. Big institutional serial, such equally from the Cleveland Clinic, accept reported repair rates of 99.5% in near 1,000 patients. Even early in robotic series, repair rates for degenerative pathology have been in backlog of 98% (9,21,22).
Against this background, frequency of reinterventions for repair failures have reduced as centre experience increases and the learning curve is traversed. Chitwood et al. described an initial 7% reoperation rate for repair failure in the first 100 cases which subsequently dropped to 4.v% in the following 200 cases (23). Spud et al. besides reported a fall in repeat mitral reinterventions over v years in 1,257 patients (16). During the first one-half of their written report, reintervention rates were 6.8% dropping to 0.9% in the latter half and, in 91% of cases, information technology was possible to redo the procedure robotically. Reported v-year freedom from reoperations of 93.8% and 97.7%, and 5- and vi-yr freedom from ≥2+ recurrent MR of 94.six% and 85% respectively provide evidence for immovability of repair (sixteen,24).
Operative durations
Longer cardiopulmonary featherbed (CPB) fourth dimension, aortic cross clamp (90) and total operative times for robotic mitral repair in comparing to both sternotomy and mini-thoracotomy are a frequent finding in all analyses. Although operative times decrease with increasing experience (20,25,26), this is often kickoff by increasing operative complexity as confidence with the technique develops (27).
Techniques to reduce operative times have targeted endoscopic knot tying every bit i of the more labour intensive aspects of the procedure. Delegating this task to the bedside surgeon, rather than tying endoscopically with the robot, saves considerable fourth dimension. A continuous running suture technique for annuloplasty band insertion, and pre-tied knots for atrial closure, has demonstrated a median 32-minute reduction in CPB and nineteen-infinitesimal reduction in cross clamp time (28). Some adaptations were less favourable, for example, the utilize of nitinol clips to secure annuloplasty bands. This resulted in a higher rate of ring dehiscence and was subsequently abandoned. The advent of automatic titanium clip knot fasteners (Cor-Knot®, LSI Solutions, Victor, NY, U.s.) has been demonstrated to save over twenty minutes of ischemic time in both mini mitral and robotic surgery (29).
Conversion to sternotomy
Almost all successful robotic programmes have surgical teams highly experienced at mini mitral surgery, having performed several hundred of these earlier adopting robotic engineering science, and we would see this as a pre-requisite to starting a robotic plan. Conversion to sternotomy can often be avoided past undocking the robot and extending the access port past 2 cm and completing the procedure as a mini mitral procedure thus nonetheless retaining a less invasive approach. Need for conversion from robotic access can exist seen to reduce equally feel is gained, with conversion occurring in 5–9.ane% during the early part of the learning curve, compared to 0.7–1.3% afterwards on (xvi,26,xxx). Conversion can occur for many reasons, such as instrument conflicts, bleeding, or concerns with aortic apoplexy/myocardial protection. Robotic system malfunctions are rare only take been reported (sixteen,23,26,31).
Morbidity
Most comparative series of robotic mitral surgery have demonstrated either a reduced or equal complexity rate compared to sternotomy cases with a reduced length of ICU and hospital stay, and faster return to normal activities (14,23,25,32,33). Wound infections are extremely rare with mini-thoracotomy approaches. 1 disadvantage, described in an STS database review past Gammie et al. exploring less invasive mitral surgery (robotic and mini mitral) versus sternotomy, was a higher charge per unit of cerebrovascular accident (CVA), which has been attributed to retrograde femoral arterial perfusion. This reported an odds ratio of 1.96, suggesting nigh double the risk of CVA with less invasive techniques (34). Withal, on closer examination, a multitude of confounding factors obfuscated interpretation of Gammie's data including:
- Imprecise definitions of minimally invasive mitral valve surgery;
- The issue of the substantial learning bend;
- Retrospective comparisons of small celebrated cohorts with baseline differences and differing risk profiles for atherosclerosis;
- Different methods of aortic occlusion and
- Lack of reporting of peripheral vascular illness (PVD) or aortic assessment in patient populations (35).
It is also important to notation in Gammie'due south assay that the median number of less invasive mitral cases per US middle per year was iii. We take learned from Prof. Mohr's group in Leipzig that minimally invasive mitral surgery is an operation with a long learning bend (75–125 cases) with better results accomplished in surgeons performing >1 case per week (36). Thus, at a rate of iii cases per yr, it would have simply 1 surgeon in each unit of measurement a whole career to traverse the learning bend. Assessing results of a procedure performed past surgeons even so in their learning curve volition conspicuously bias the results. In all other analyses, including in patients older than 65 years, no significant difference has been demonstrated between stroke rates in robotic and sternotomy approaches (25,26).
Length of ICU and hospital stay have consistently plant in favour of robotic techniques, fifty-fifty when compared to a video-assisted approach. The hospital stay is consistently ane–2 days shorter with fewer ventilated hours and before ICU discharge (14,25,33,37). White potato et al., in a series of 1,257 robotic mitral valve surgeries, reported a mean length of hospital stay of 4.nine±iv.4 days with 37% patients existence discharged within 4 days (16). This also translates into earlier render to paid employment on discharge (38).
The data for rates of blood transfusion and atrial fibrillation (AF) comparing robotic surgery to sternotomy is alien, with some reports suggesting a lower incidence of these (20) and others showing no difference (22,26). Similarly, other reports have shown higher rates of these with robotic surgery than with the mini approach (25) whereas others have shown no departure (26).
Disadvantages
Costs and the learning bend
Without incertitude the initial costs of developing a robotic programme are significant with the initial capital outlay followed by ongoing costs of the annual maintenance contract and instruments. Operative times are longer leading to fewer patients going through the operating suite on a daily basis offset by the increased volume of referrals that robotic surgery attracts. Data from the Cleveland Clinic shows that the learning bend is significant, with the greatest reduction in operative times occurring during the first 200 cases with simply pocket-sized reductions beyond this (19,39).
Paul et al. showed equivalent costs in 631 propensity matched pairs of patients from the National Inpatient Sample from 2008 to 2022 undergoing either robotic or sternotomy mitral valve repair (xiv). However, their data did non include the toll of the robotic system, maintenance and acquittal. Coyan et al. did account for robotic capital depreciation and instrumentation costs, and showed no significant differences in total costs of robotic mitral operations compared to a propensity matched group of sternotomy operations ($27,662 vs. $28,241, P=0.27, respectively) (33). Early on direct costs were higher in the robotic group, counterbalanced by higher late indirect costs in the sternotomy cohort, related to increased length of stay, transfusion requirements and readmission rates.
Using calculations taking into business relationship buy costs and maintenance as well every bit disposables, Mihaljevic et al. compared the economic benefits of robotic mitral repair versus alternative admission via sternotomy, partial sternotomy and anterolateral thoracotomy using propensity matching (38). Income from return to paid employment as well every bit costs of postoperative care were considered. Overall costs for robotic procedures were between 14–16% greater than alternative surgical techniques. However, with cost projection it was possible to place that in centres performing 55–100 cases per year, this would equilibrate over time with other techniques. In the majority of institutions, capital costs of the robot are spread across multiple surgical specialties and thus smaller volume robotic cardiac surgery programmes can still exist economically viable (40). Regardless of how the upper-case letter cost is rationalized, information technology is unfair from an economic standpoint to consider this in a cost effectiveness analysis. The purchase of a robot is a sunk cost, meaning a cost that has already been incurred and cannot exist recovered, in much the same mode as is the cost of edifice a hybrid operating room to facilitate transcatheter aortic valve replacement (TAVR). Every bit Halkos argues, the cost of the hybrid room is non incorporated into analyses when comparing TAVR to surgical aortic valve replacement (AVR), so why should robotic mitral valve repair be held to a different standard (twoscore)?
Case volume is fundamental to the success of a robotic mitral valve repair programme, not but for fiscal reasons but likewise the ability to successfully navigate the learning bend. Lessons from experienced centres highlight that expert leadership and a dedicated team are vital and recommend a minimum number of 20 cases per year to maintain proficiency (41). As instance selection is vital during the learning curve, just high volume centres take the caseload to do this in a temporally efficient manner. Detractors comment that there is a disparity in the frequency of robotic procedures existence performed in centres that accept the resources, given that few perform greater than 30 robotic cases per twelvemonth (42).
Lack of tactile feedback
In our feel, visual clues such every bit tissue deformation provide adequate information. Reiley et al. demonstrated that visual strength feedback primarily benefits novice robot-assisted surgeons with diminishing benefits amongst experienced surgeons (43).
Technical considerations—tips and tricks to shorten the learning curve
The techniques of robotic mitral valve repair have been extensively described elsewhere, so nosotros would like to share the pearls and pitfalls that nosotros have learned, and those which we feel are near of import in the successful implementation of a robotic programme.
Training and teamwork
A team arroyo is vital to robotic surgery and this must exist planned as conscientiously as the equipment from the inception of the programme. The panel surgeon should exist a loftier volume mini-mitral surgeon who has followed the Intuitive Surgical training pathway. Sitting at the console for the outset time is not the fourth dimension to be learning mitral valve repair or the nuances of managing CPB and myocardial protection from the correct minithoracotomy approach. The anaesthetist should be skilled at 3D transoesophageal echocardiography and jugular drainage cannula insertion. Whether the bedside assistant is a second surgeon, fellow or surgical assistant needs to be decided early, and the whole team needs to train together, both by visiting other established robotic programmes and performing wet labs and multiple dry runs. The surgeon who accepts the team for case observation should be the proctor for the first five cases. All the manoeuvres inside the center should exist practiced on latex models and/or pig hearts. With the surgeon at the panel, the patient-side assistant and the scrub nurse need to be able to troubleshoot instrument conflicts and tie intra-corporeally. Both scrub nurse and circulating nurse should be familiar with mini mitral surgery. Communication must be clear given at that place is reliance from the panel surgeon on the patient-side team. Wireless headsets improve the quality of communication between team members and reduce elevation noise levels in the robotic operating room (44). Recognition of this difference in team dynamics means that in our institution at that place has been an emphasis on inclusion of all operating room staff in preparation with a low authorization slope, so all team members are empowered to speak up at any time.
Patient and port-positioning
The right chest is elevated by thirty° with a eternalize nether the right scapula and it is important that this is placed sufficiently caudad so that the head of the right humerus tin can fall posteriorly, helping to create room for the left arm port (threerd intercostal infinite). A long port may exist needed in large patients.
Make sure the centre mail service of the patient cart is level with the camera port—if too caudal, arms 3 and iv both lie likewise flat and conflict externally. The admission port and camera port both become in the same intercostal infinite, normally the fourth. Occasionally, it may be the 3rd interspace in patients with a brusque chest cavity from cranial to caudal. We accept found that a reliable indicator of the correct interspace is that overlying the right junior pulmonary vein on the chest X-ray.
The correct arm port goes 2 interspaces caudal to the access port in the anterior axillary line. Left lateral rolling of the table will preclude conflict of the elbow of the right arm with the left iliac crest. The left atrial retractor port goes in the 4th or 5th interspace, medial to the midclavicular line.
Cannulation
Our preference is always to use an internal jugular drainage cannula in all patients equally adequate venous drainage is never an issue. Remember that poor venous drainage will compromise correct heart protection. Positioning the inferior vena cava (IVC) cannula into the superior vena cava (SVC) to deed like a rod passing through the right atrium improves the valve exposure when the robotic left atrial retractor is deployed. A potent venous cannula (eastward.g., Biomedicus, Medtronic, Dublin, Ireland) therefore has advantages over more flexible ones (e.g., Estech dual stage).
CPB and myocardial protection
Operative times will be prolonged during the learning bend, then systemic cooling to 28–xxx °C is of import for both myocardial protection and protection of the right lung to avoid unilateral pulmonary edema (45). Unilateral pulmonary edema is probably an ischemia-reperfusion injury of the correct lung, occurs in <ane% of cases and is associated with a 33% bloodshed. Minimising the duration of single lung ventilation, maintenance of systemic force per unit area on CPB ≥65 mmHg, minimising anaemia and agile cooling on CPB are important preventative measures.
Myocardial protection with single dose cardioplegia (eastward.yard., Custodiol® or del Nido) is helpful to avoid redosing. Additionally, crystalloid cardioplegia fits well with IntraClude utilise as the line pressures are lower during infusion than when blood cardioplegia is used. Beware, yet, of repeated saline testing washing the cardioplegia out and compromising myocardial protection.
Intraclude or transthoracic clench
There are, broadly speaking, two techniques for robotic mitral valve surgery based on the technique of aortic occlusion. The LEAR technique (Lateral Endoscopic Arroyo for Robotics) was developed by Dr. Douglas Murphy (Atlanta, Us) and is a port-based totally endoscopic approach using 4 8-mm ports and one 20-mm flexible access port (16). With a port-based approach, placing a cannula in the aortic root becomes challenging so an endoaortic balloon is used to occlude the aorta (IntraClude, Edwards Lifesciences, Irvine, CA, United states of america). This is the least invasive option but has the merchandise-off of calculation an extra layer of complexity in the positioning and direction of the IntraClude to ensure adequate aortic occlusion and myocardial protection is maintained. Deployment of the endoballoon is like flight a kite in the current of air, its position being dependent on the pressure level in the aorta balanced by the tension on its catheter. Therefore, bilateral radial arterial cannulae are required to detect distal migration which would occlude the origin of the innominate artery (east.g., if the systemic blood pressure falls). Constant vigilance is required.
One innovative development to help with IntraClude placement is the use of an albumin and indocyanine light-green (ICG) solution to fill up the balloon. This fluoresces with the firefly fluorescence imaging of the da Vinci system allowing real-time, prototype-guided placement of the IntraClude (Figure iv) (46). Disadvantages of the IntraClude include that it is unmarried use and expensive (£1,500). When this is added to the boosted cost of the robotic procedure, where each of the 5 instruments has a limit of 10 uses (approx. £200 per use, thus an additional £ane,000 per instance), conscientious consideration needs to be given to the cost: benefit ratio in healthcare systems with constrained resources. There is besides a learning bend for the IntraClude, and information technology is not wise to permit the learning curve of robotic surgery to overlap that of the IntraClude.
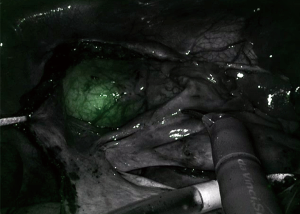
Figure four Indocyanine green fluorescing in the IntraClude in the mid ascending aorta.
The culling technique popularised past Dr. Randolph Chitwood (Greenville, NC, USA) uses a 4-cm minithoracotomy, through which the 3D scope is placed, and three 8-mm ports. A transthoracic clamp (Chitwood clamp) is used to occlude the aorta. This has the advantage that information technology does not migrate, provides reliable aortic occlusion and, as information technology is reusable, is more than cost effective. Smaller femoral cannulae can be used as in that location is no demand to accommodate the catheter of the IntraClude, arterial line pressures are lower and bilateral femoral cannulation is consequently rarely needed. This provides a pregnant cost saving and chiefly makes the overall process less complex merely does take some disadvantages. Firstly, a minithoracotomy is needed rather than a truly port-based approach; secondly, at that place is the potential for conflict between the clamp and the left robotic arm and thirdly, it necessitates a twond bypass run to decannulate and control the root of the aorta, which can occasionally lead to troublesome bleeding.
Repair technique
If the valve repair looks more complex than initially predictable, undock the robot, return to the tableside, extend the incision by one–ii cm, and proceed as a mini mitral. Never compromise on quality of the repair. Using the tableside banana to tie the knots saves time; Cor-Knot® also saves time. Most surgeons use flexible bands rather than rings with robotics, simply information technology is perfectly possible to place a semi-rigid band or ring with the robot. Utilize pre-knotted sutures for left atrial closure to save further time (Effigy v).
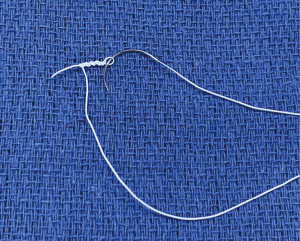
Effigy five Pre-knotted suture, fabricated by knotting a CV4 GoreTex suture over a nerve hook.
Patient selection
The surgical approach (robot vs. mini vs. sternotomy) should be tailored both to the patient and the experience of the surgical team using the following rules:
- Safe must never be compromised;
- Repairability of the valve should never be compromised;
- These are both achieved in the least invasive mode possible.
For the get-go five cases, the ideal patients are slim males with large femoral vessels and isolated posterior leaflet prolapse with some excess tissue. Exclusion criteria vary with experience and are more than stringent at the offset of the programme. Some consider pre-operative aortoiliac contrast-enhanced CT important for operative planning. This assesses for atherosclerotic burden with some testify that it is associated with a reduced chance of stroke (35,47) but besides identifies arterial/venous anatomy, besides every bit obliquity of the ribs which has implications for port placement. The Cleveland Clinic grouping take documented a thorough listing of exclusion criteria as follows: aortic regurgitation, mitral annular calcification, reoperation, left ventricular (LV) dysfunction/dilatation, severe pulmonary hypertension, aortoiliac atherosclerosis, femoral avenue diameter <7 mm, and pectus excavatum (19).
Still, it must not be forgotten that the patients who are going to gain the well-nigh benefit from less invasive techniques are the highest chance patients, those who tolerate the conventional surgical trauma least well. An all-encompassing listing of exclusion criteria volition deny many patients the benefits of robotic surgery. Every bit experience with the robotic platform increases, many of these get relative, e.g., axillary cannulation can exist used when the thoracic or intestinal aorta has grade V atheroma or the femoral arteries are small, and reoperations are technically easier and safer through the correct chest after prior sternotomy.
Conclusions
Totally endoscopic robotic mitral valve repair, performed in high-volume centres by high-volume surgeons, represents the least invasive form of surgical therapy for mitral valve affliction. This leads to a rapid render to normal activities, with proven mid-term durability and prognostic advantage. When one weighs this confronting the uncertain durability and residual MR associated with transcatheter repairs, it becomes articulate that robotic techniques will be a major hurdle lying in the pathway of the inexorable advance of transcatheter techniques. As experience grows with robotic techniques and more than cardiac surgeons get proficient with this innovative technology, the volume of robotic cardiac procedures effectually the world will increase helped by the introduction of new robotic systems and patient demand. Well informed patients will increasingly seek out the opportunity of robotic valve reconstruction in reference centres in the hands of a few highly experienced robotic surgeons.
Acknowledgments
Funding: None.
Provenance and Peer Review: This article was commissioned by the Invitee Editors (Jason Ali and Yasir Abu-Omar) for the series "Minimally Invasive Cardiac Surgery" published in Journal of Thoracic Affliction. The article has undergone external peer review.
Peer Review File: Bachelor at http://dx.doi.org/10.21037/jtd-20-1790
Conflicts of Involvement: All authors take completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1790). The series "Minimally Invasive Cardiac Surgery" was commissioned past the editorial office without whatsoever funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are answerable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any office of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the not-commercial replication and distribution of the commodity with the strict proviso that no changes or edits are made and the original piece of work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Beckmann A, Meyer R, Lewandowski J, et al. German Heart Surgery Written report 2022: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg 2022;67:331-44. [Crossref] [PubMed]
- Cheng DC, Martin J, Lal A, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations (Phila) 2022;6:84-103. [Crossref] [PubMed]
- Cao C, Gupta Due south, Chandrakumar D, et al. A meta-analysis of minimally invasive versus conventional mitral valve repair for patients with degenerative mitral illness. Ann Cardiothorac Surg 2022;2:693-703. [PubMed]
- Modi P, Hassan A, Chitwood WR Jr. Minimally invasive mitral valve surgery: a systematic review and meta-assay. Eur J Cardiothorac Surg 2008;34:943-52. [Crossref] [PubMed]
- Sundermann SH, Sromicki J, Rodriguez Cetina Biefer H, et al. Mitral valve surgery: right lateral minithoracotomy or sternotomy? A systematic review and meta-assay. J Thorac Cardiovasc Surg 2022;148:1989-1995.e4. [Crossref] [PubMed]
- Glauber M, Miceli A, Canarutto D, et al. Early on and long-term outcomes of minimally invasive mitral valve surgery through correct minithoracotomy: a 10-year experience in 1604 patients. J Cardiothorac Surg 2022;ten:181. [Crossref] [PubMed]
- Carpentier A, Loulmet D, Aupecle B, et al. Computer assisted open up heart surgery. Beginning case operated on with success. C R Acad Sci III 1998;321:437-42. [Crossref] [PubMed]
- Mohr FW, Falk V, Diegeler A, et al. Computer-enhanced coronary avenue bypass surgery. J Thorac Cardiovasc Surg 1999;117:1212-4. [Crossref] [PubMed]
- Chitwood WR Jr, Nifong LW, Elbeery JE, et al. Robotic mitral valve repair: trapezoidal resection and prosthetic annuloplasty with the da vinci surgical system. J Thorac Cardiovasc Surg 2000;120:1171-2. [Crossref] [PubMed]
- Grossi EA, Lapietra A, Applebaum RM, et al. Case study of robotic instrument-enhanced mitral valve surgery. J Thorac Cardiovasc Surg 2000;120:1169-71. [Crossref] [PubMed]
- Nifong LW, Chu VF, Bailey BM, et al. Robotic mitral valve repair: experience with the da Vinci system. Ann Thorac Surg 2003;75:438-42; discussion 443. [Crossref] [PubMed]
- Nifong LW, Chitwood WR, Pappas PS, et al. Robotic mitral valve surgery: a United States multicenter trial. J Thorac Cardiovasc Surg 2005;129:1395-404. [Crossref] [PubMed]
- Pettinari Grand, Navarra E, Noirhomme P, et al. The state of robotic cardiac surgery in Europe. Ann Cardiothorac Surg 2022;6:1-viii. [Crossref] [PubMed]
- Paul S, Isaacs AJ, Jalbert J, et al. A population-based analysis of robotic-assisted mitral valve repair. Ann Thorac Surg 2022;99:1546-53. [Crossref] [PubMed]
- Cao C, Wolfenden H, Liou G, et al. A meta-analysis of robotic vs. conventional mitral valve surgery. Annals of cardiothoracic surgery 2022;4:305-14. [PubMed]
- Tater DA, Moss E, Binongo J, et al. The Expanding Role of Endoscopic Robotics in Mitral Valve Surgery: 1,257 Consecutive Procedures. Ann Thorac Surg 2022;100:1675-81; discussion 1681-2. [Crossref] [PubMed]
- Nifong LW, Rodriguez E, Chitwood WR Jr. 540 consecutive robotic mitral valve repairs including concomitant atrial fibrillation cryoablation. Ann Thorac Surg 2022;94:38-42; word 43. [Crossref] [PubMed]
- Tarui T, Ishikawa N, Horikawa T, et al. Get-go Major Clinical Outcomes of Totally Endoscopic Robotic Mitral Valve Repair in Japan- A Single-Heart Experience. Circ J 2022;83:1668-73. [Crossref] [PubMed]
- Gillinov AM, Mihaljevic T, Javadikasgari H, et al. Early results of robotically assisted mitral valve surgery: Analysis of the first m cases. J Thorac Cardiovasc Surg 2022;155:82-91.e2. [Crossref] [PubMed]
- Hawkins RB, Mehaffey JH, Mullen MG, et al. A propensity matched analysis of robotic, minimally invasive, and conventional mitral valve surgery. Heart 2022;104:1970-5. [Crossref] [PubMed]
- Murphy DA, Miller JS, Langford DA, et al. Endoscopic robotic mitral valve surgery. J Thorac Cardiovasc Surg 2006;132:776-81. [Crossref] [PubMed]
- Suri RM, Burkhart HM, Daly RC, et al. Robotic mitral valve repair for all prolapse subsets using techniques identical to open valvuloplasty: establishing the benchmark against which percutaneous interventions should be judged. J Thorac Cardiovasc Surg 2022;142:970-ix. [Crossref] [PubMed]
- Chitwood WR Jr, Rodriguez E, Chu MW, et al. Robotic mitral valve repairs in 300 patients: a unmarried-middle feel. J Thorac Cardiovasc Surg 2008;136:436-41. [Crossref] [PubMed]
- Suri RM, Taggarse A, Burkhart HM, et al. Robotic Mitral Valve Repair for Simple and Complex Degenerative Affliction: Midterm Clinical and Echocardiographic Quality Outcomes. Circulation 2022;132:1961-8. [Crossref] [PubMed]
- Wang A, Brennan JM, Zhang Southward, et al. Robotic Mitral Valve Repair in Older Individuals: An Assay of The Society of Thoracic Surgeons Database. Ann Thorac Surg 2022;106:1388-93. [Crossref] [PubMed]
- Mihaljevic T, Jarrett CM, Gillinov AM, et al. Robotic repair of posterior mitral valve prolapse versus conventional approaches: Potential realized. J Thorac Cardiovasc Surg 2022;141:72-80.e4. [Crossref] [PubMed]
- Charland PJ, Robbins T, Rodriguez E, et al. Learning curve analysis of mitral valve repair using telemanipulative applied science. J Thorac Cardiovasc Surg 2022;142:404-ten. [Crossref] [PubMed]
- Mihaljevic T, Jarrett CM, Gillinov AM, et al. A novel running annuloplasty suture technique for robotically assisted mitral valve repair. J Thorac Cardiovasc Surg 2022;139:1343-4. [Crossref] [PubMed]
- Perin G, Shaw Grand, Pingle V, et al. Use of an automatic knot fastener shortens operative times in minimally invasive mitral valve repair. Ann R Coll Surg Engl 2022;101:522-8. [Crossref] [PubMed]
- Javadikasgari H, Suri RM, Tappuni B, et al. Robotic mitral valve repair for degenerative posterior leaflet prolapse. Ann Cardiothorac Surg 2022;6:27-32. [Crossref] [PubMed]
- Cheng West, Fontana GP, De Robertis MA, et al. Is robotic mitral valve repair a reproducible approach? J Thorac Cardiovasc Surg 2022;139:628-33. [Crossref] [PubMed]
- Folliguet T, Vanhuyse F, Constantino Ten, et al. Mitral valve repair robotic versus sternotomy. Eur J Cardiothorac Surg 2006;29:362-6. [Crossref] [PubMed]
- Coyan G, Wei LM, Althouse A, et al. Robotic mitral valve operations by experienced surgeons are price-neutral and durable at ane twelvemonth. J Thorac Cardiovasc Surg 2022;156:1040-seven. [Crossref] [PubMed]
- Gammie JS, Zhao Y, Peterson ED, et al. Less-Invasive Mitral Valve Operations: Trends and Outcomes From The Society of Thoracic Surgeons Adult Cardiac Surgery Database. The Annals of Thoracic Surgery 2022;90:1401-10.e1. [Crossref] [PubMed]
- Modi P, Chitwood WR Jr. Retrograde femoral arterial perfusion and stroke risk during minimally invasive mitral valve surgery: is in that location cause for concern? Ann Cardiothorac Surg 2022;2:E1 [PubMed]
- Holzhey DM, Seeburger J, Misfeld M, et al. Learning minimally invasive mitral valve surgery: a cumulative sum sequential probability analysis of 3895 operations from a unmarried high-volume eye. Apportionment 2022;128:483-91. [Crossref] [PubMed]
- Kam JK, Cooray SD, Kam JK, et al. A cost-analysis study of robotic versus conventional mitral valve repair. Eye Lung Circ 2022;19:413-8. [Crossref] [PubMed]
- Mihaljevic T, Koprivanac M, Kelava M, et al. Value of robotically assisted surgery for mitral valve disease. JAMA Surg 2022;149:679-86. [Crossref] [PubMed]
- Goodman A, Koprivanac M, Kelava One thousand, et al. Robotic Mitral Valve Repair: The Learning Curve. Innovations (Phila) 2022;12:390-7. [Crossref] [PubMed]
- Moss Eastward, Halkos ME. Price effectiveness of robotic mitral valve surgery. Ann Cardiothorac Surg 2022;6:33-vii. [Crossref] [PubMed]
- Rodriguez East, Nifong LW, Bonatti J, et al. Pathway for surgeons and programs to found and maintain a successful robot-assisted adult cardiac surgery program. J Thorac Cardiovasc Surg 2022;152:9-xiii. [Crossref] [PubMed]
- Robicsek F. Robotic cardiac surgery: time told! J Thorac Cardiovasc Surg 2008;135:243-vi. [Crossref] [PubMed]
- Reiley CE, Akinbiyi T, Burschka D, et al. Furnishings of visual strength feedback on robot-assisted surgical task performance. J Thorac Cardiovasc Surg 2008;135:196-202. [Crossref] [PubMed]
- Tsafrir Z, Janosek-Albright K, Aoun J, et al. The impact of a wireless audio organisation on communication in robotic-assisted laparoscopic surgery: A prospective controlled trial. PLoS One 2022;15:e0220214 [Crossref] [PubMed]
- Moss E, Halkos ME, Binongo JN, et al. Prevention of Unilateral Pulmonary Edema Complicating Robotic Mitral Valve Operations. Ann Thorac Surg 2022;103:98-104. [Crossref] [PubMed]
- Yaffee DW, Loulmet DF, Fakiha AG, et al. Fluorescence-guided placement of an endoaortic balloon occlusion device for totally endoscopic robotic mitral valve repair. J Thorac Cardiovasc Surg 2022;149:1456-8. [Crossref] [PubMed]
- Leonard JR, Henry Chiliad, Rahouma M, et al. Systematic preoperative CT scan is associated with reduced adventure of stroke in minimally invasive mitral valve surgery: A meta-analysis. Int J Cardiol 2022;278:300-6. [Crossref] [PubMed]
Cite this commodity as: Toolan C, Palmer K, Al-Rawi O, Ridgway T, Modi P. Robotic mitral valve surgery: a review and tips for safely negotiating the learning curve. J Thorac Dis 2022;13(3):1971-1981. doi: 10.21037/jtd-twenty-1790
Source: https://jtd.amegroups.com/article/view/45078/html
Posted by: mullinspriont.blogspot.com


0 Response to "What Are The Requirements For A Patient To Have Robotic Mitral Valve Repair"
Post a Comment